|
|
| |
ARTICLES
Microsurgery: A NEW TECHNIQUE FOR TREATMENT OF DISEASES congenital,
acquired and Trauma AVAILABLE IN ECUADOR.
Dr. Walter
Francis Huaraca.
Plastic Surgeon - microsurgeon.
Specialized in Brazil.
Prof. Dr. Fausto Viterbo.
Head of service discipline of Plastic Surgery - Microsurgery of the
Paulista State University, Botucatu, Brazil.
Dr. Jacqueline Freire Freire.
Resident clinical Samborondon Kennedy.
History:
In 1921 a Swiss named Nylen otolaryngologist performed an operation
in the inner ear with a surgical microscope. Carl Zeiss in 1953
began the mass production of surgical microscopes.
The first transfer of free flap was first described by Daniel and
Taylor in 1973 revolutionized reconstructive surgery and
microcirugía.1 In Latin America, Brazil was the pioneer where
transposition was performed the first microsurgical and today are
still performing surgical procedures complex as liver
transplantation among others.
This type of complex microsurgical procedures are performed in major
countries like USA, France, Spain, Taiwan, Japan, Brazil and now is
available in our country.
Summary:
Microsurgery is an important technique in plastic surgery enables
the surgeon experienced in microsurgery to repair any defects in the
body, be it congenital, acquired or traumatic. It can be applied
safely in adults and children.2
The success of these microsurgical procedures lie in the
preoperative planning, which is a significant task and will have
direct bearing on the outcome of the proceedings, the patient
selection, surgical planning, site selection donor tissue viability
and technical aspects transferred of microvascular anastomosis are
very important, however an error in one of these aspects will lead
to the failure of free flap. There are some factors such as age,
patients undergoing radiation therapy, chemotherapy and several
systemic diseases such as atherosclerosis, diabetes, cardiovascular
limiting their aplicación.3-4
Keywords:
Microsurgery, free flaps, autologous tissue Reinplantes, plastic
surgery reconstructive surgical procedures.
Microsurgery is the most important breakthrough occurred in plastic
surgery, this technique allows tissue transfers (dermal,
myocutaneous, osteomyocutaneous) safely.
INTRODUCTION:
Microsurgery is an important technique in plastic surgery, this
procedure allows for reimplantation of fingers, arms, legs, penis,
ears, face, digital downloads toe to the hand, lower limb
revascularization at tibiofibular trunk or tibial anterior.5-6-7-8
enables still free flap transposition (muscle, bone or soft tissue)
for correction of major congenital abnormalities, post-traumatic and
post-tumor resection that were previously considered inoperable due
to the complexity of injuries and depth. 9-10-11-12-13-14 With this
tool we are able to perform various reconstructive procedures and
make the area coverage bloody head, neck, chest, pelvic limb or any
other area that needs coverage for a defect caused by an accident as
brachial plexus palsy or disfiguring disease such as facial palsy or
soft tissue cancer. Currently all of these disorders can be treated
safely with new and efficient techniques of reconstruction, these
free flaps (Free flap) are intimately attached to its vascular
pedicle consisting of arteries, veins, which need blood supply for
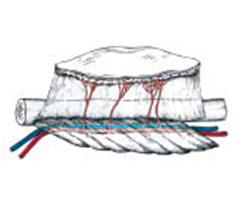
survival. Graphic: 1, Photo 1
 |
|
Figure 1 - Fibula free flap osteomyocutaneous, which
is in close relationship with its vascular pedicle
(artery and vein). |
The dissections
were performed with the aid of a microscope or magnifying lenses
called loupes. (Photos 2-3). This is achieved with a better
technique in the management structures and with less damage to
tissues.
Is essential to have proper equipment such as mini clamps, needle
holders, scissors, clamps and so on. This instrument is delicate and
difficult to manufacture in many countries of America (photo 2,3,4).
What is a free flap?
It is the well-vascularized tissue transfer are these skin,
myocutaneous, osteomyocutaneous to anywhere in the body, a vascular
pedicle (artery vein nerve) that guarantees the survival of
colgajo.1-13
Materials and Methods:
This work was performed at the Hospital of the Paulista State
University, Botucatu (Brazil) and Cosmetic Surgery Clinic, Dr.
Fausto Viterbo Microsurgery, during the period of 16 April 2008 -
March 31, 2010.
Reconstructions were performed for various diseases using free
flaps, the flaps were used more latissimus dorsi muscle, gracilis
muscle, fibula flap of osteomyocutaneous, skin flap DIEP.15 Each
procedure has its indications, and the ideal choice of technique
depends on individual factors such as : age, health status,
anatomical characteristics, presence of associated conditions,
assessment of damage and the tissue conditions by transplantar.14-16
These microsurgical procedures performed by plastic surgeon trained
in microsurgery, prepares blood vessels in the recipient area and
donor, then with the aid of a microscope or magnifying glass,
connecting the arteries and veins of the transplanted tissue to the
area to rebuild.
Advantages of free flaps:
1 .- Provides security and full coverage of large defects in the
body caused by various diseases
2 .- Less surgical procedures to achieve a satisfactory result.
2.-The possibility of transferring specific tissues according to the
needs of each patient. bone, muscle, skin, mucous membranes or
different combinations, achieving better results.1-16
Results:
This type of microsurgical procedures should be performed in
hospitals that provide security guarantees for the patient and have
the necessary equipment and microscopes for microsurgery
appropriate. Photos :2-3-4.
In all operated cases had favorable, according to plan, we obtained
a success rate of 95%. Photos: 5-9
There were small contingencies as dermoepidermolisis, photo 6 in
such cases conservative treatment was performed healings.
 |
|
Figure 2: Free flap. The deep inferior epigastric
perforator (DIEP) flap for breast reconstruction. |
Discussion:
These microsurgical interventions are performed in a single
surgical, two surgical teams need to shorten the operating time.
Each microsurgery is a surgical time average of 6 -10 to 12
hours depending on what type of surgery accordingly. This found
that the use of the microscope improves the quality of
anastomosis in relation to use of magnifiers.
The choice of recipient vessels is very important, because they
possess identical vascular diameters and its proximity to the
area to rebuild. The dissection and preparation of the vessels
must be very sensitive and accurate, because the vascular
endothelium is injured very easily, compression and / or
excessive tension leads to vascular spasm which can result in
thrombosis. Another factor to consider is the length of the
vascular pedicle, if this is too short causes tension on the
anastomosis, we must also avoid redundancy in length which can
cause twisting and compression of the pedicle leading to loss of
flap.
The use of saphenous vein grafts and recipient vessels between
the free flap should be used with caution because potentiates
thrombosis of the vessels. Vascular thrombosis in most cases is
technical error in the anastomosis and / or use of a glass with
the injured endothelium. The type of anastomosis used is termino-lateral
and / or end to end, the latter presenting greater
effectiveness. When we are faced with an imbalance in the
diameter of the vessels should be performed
end-to-lateral.17-18-19-20 is considered microanastomosis
process is the most important determinant of vessel patency.
The flap ischemia time is the amount of time that passes from
the free flap vascular pedicle is severed from the donor area to
be anastomosed in the recipient vessels and restore blood flow.
The ideal time for this procedure is up to 4 hours in skin flaps
and myocutaneous, while up to 6 hours in free flaps
osteomiocutáneos.21-22-23-24-25
The medication is added in the immediate postoperative heparin
is the use of low molecular weight sodium 5,000 IU. subcutaneous
c / day for 3-5 days during their hospitalization, subsequently
added to treatment with pentoxifylline or aspirin.
Close monitoring is performed in the post-surgery in order to
identify any changes in the hemodynamics of the flap. Caution
should be exercised after 20 minutes post-anastomosis, the next
critical period is 24-72 hours, the success of a free flap is to
reach the 5 days without filing trombosis.26-27-28-29- 30-31-32
-
In some countries, and other hospitals recommend performing
vascular pedicle control by using color Doppler ultrasound every
2 hours during the first 12 hours, then every 6 hours to
complete the 72 hours. 33-34
Conclusions:
The use of microsurgical flaps is safe, effective, it is
performed in an operating time can be applied in adults and
children allowing tissues to restore large areas of previously
inoperable with good results, improving the quality of life for
these patients. Reconstructions also allows functional and
aesthetic results with minimal commitment from the donor area.
References:
1 .- Daniel RX, Taylor GL: Distant transfer of an island flap by
microvascular anastomoses: a clinical technique. Plast Reconstr
Surg 52: 111-117, 1973
2.-Joseph Upton, M.D. Free-Tissue Transfer Pediatric Plastic and
Reconstructive Surgery • December 2009.
3. Bernstein EF, Sullivan FJ, Mitchell JB, et al. Biology of
chronic radiation effect on wound healing and Tissues. Clin
Plast Surg. 1993, 20:435-451.
4. Drake DB, Oishi SN. Wound healing in chemotherapy
Considerations
and radiation therapy. Clin Plast Surg. 1995, 22:31-37.
5 .- Fernandez.R. Free flaps in mandibular reconstruction Oral
Maxillofacial Surg Clin Atlas N Am 14 (2006) 143-150
6 .- Donnal Serafin, Atlas of Microsurgical Composite Tissue
Transplantation. Illustrated by Robert G. Gordon 1996. Flap, p.
191-204. The Fibula flap, p. 547-574.
7 .- Donnal Serafin, Atlas of Microsurgical Composite Tissue
Transplantation The musculocutaneous Latissimus Muscle Dorsis
Illustrated by Robert G. Gordon 1996. Flap, p. 191-204 ..-
8 .- Rodolfo Chedid, craniofacial com Reconstrução
microcirúrgicos retalhos Rev. Bras. Cir. Cabeça Pescoço, v. 38,
No. 2, p. 103-107, April / May / Junho 2009
9 .- I Pinho S. Dias Reimplantation of upper Membros: case
studies of 23 years. Brazilian Journal of Plastic Surgery Vol
24-No 3 / 2009. Pag.80
10 .- K. Souza R. Chedid Nas do retalho Versatilidade
reconstrução of cabeça forearm and pescoço: no retrospective
Análise incs. Brazilian Journal of Plastic Surgery Vol 24-No 3 /
2009. P. 3.
11 - Reis Junior Jeziorowki livre Retalho coxa Antero-lateral to
extremibades reconstrução of Brazilian Journal of Plastic
Surgery Vol 24-No 3 / 2009 .. page 79.
12 - M. Closs Groth A. Microcirúrgica Reconstrução Brasileira da
maxila.Revista of Plastic Surgery Vol 24-No 3/2009.Pag. 3529 .-
Gthot A. Duarte
13 .- Ceva Faria, A. Benedik TRAM-case report of hemangioma
livre for tramento giant. Brazilian Journal of Plastic Surgery
Vol 24-No 3 / 2009. Page 18
14 .- Glen T. Porter, MD; Microvascular Free Tissue Transfer,
Department of Otolaryngology / Head and Neck Surgery October 20,
2004
15 .- Pierre M. Chevray, MD, Ph.D., Breast Reconstruction with
Superficial Inferior epigastric Artery Flaps: A Prospective,
Comparison with TRAM and DIEP flaps, the American Society for
Reconstructive Microsurgery, in Kauai, Hawaii, on January 12,
2003.
16 .- Maurice Nahabedian., MD, FACS, * Recipient Vessel Analysis
for Microvascular Reconstruction of the Head and Neck. Annals of
Plastic Surgery • Volume 52, Number 2, February 2004.
17 .- Yamamoto Y, nohires K, Kuwahara M, et al. Superiority of
end-to-side anastomosis internal jugular vein With The: the
experience of 80 cases in head and neck microsurgical
reconstruction. Br J Plast Surg. 1999, 52: 88-91.
18 .-. Ueda K, Harii K, Nakasuka T, et al. Comparison of
end-to-end and end-to-side venous anastomosis in free-tissue
transfer Following resection of head and neck tumors.
Microsurgery. 1996, 17:146-149.
19. Bas L, May JW, Handra J, et al. End-to-end versus
end-to-side microvascular anastomosis patency in experimental
venous repairs. Plast Reconstr Surg. 1986, 77:442-450.
20 .- MF Fillinger, DB Kerns, Bruch D, et al. Does the
end-to-end anastomosis offer a functional venous Advantage over
the end-to-side venous anastomosis in high-output arteriovenous
grafts. J Vasc Surg. 1990, 12:676-688.
21 .- Rand RP Gruss JB. The saphenous arteriovenous fistula in
microsurgical
head and neck reconstruction. Am J Otolaryngol. 1994,
15:215-218.
22 .-. Sorensen JL, Muchardt O, Reumert T. Temporary
arteriovenous shunt prior to free flap transfer. Plast Reconstr
Hand Scand J Surg. 1990, 24: 43-46.
Yenidunya ..- 23 MO, Yenidunya S, Suse T, et al. Different types
of arteriovenous anastomoses femoral artery and vein entre
distal to the island groin flap. J Reconstr Microsurg. 2002,
18:301-307.
24 .-. Schultz-Mosgau S, Grabenbauer GG, Wehrhan F, et al.
Histomorphological structural Changes of Blood Vessels head and
neck pre-or after-Postoperative radiotherapy. Strahlenther Onkol.
2002, 178: 299-306.
25 .-. Hidalgo DA, Disa JJ, Cordeiro PG, et al. A review of 716
consecutive free flaps for oncologic surgical defects:
refinement in donor-site selection and technique. Plast Reconstr
Surg. 1998, 102:722-732.
26 .-. Urken ML, Weinberg H, Buchbinder D, et al. Microvascular
free flaps in head and neck reconstruction: report of 200 cases
and review of literature. Arch Otolaryngol Head Neck Surg. 1994,
120:633-640.
27 .-. Finical SJ, Doubek WG, Yogueros P, et al. The fate of
free flaps Used To
reconstruct defects in recurrent head and neck Cancers. Plast
Reconstr Surg. 2001, 107:1363-1366.
28 .- Rui Fernandes MD. Free Fibula Flap in Mandibular
Reconstruction Oral Maxillofacial Surg Clin Atlas N Am 14 (2006)
143-150.
29 .- J. Nunes Matsumoto W. Ferimento Reconstrução of Complexo
da middle third face Brazilian Journal of Plastic Surgery Vol
23-No 3 / 2008 .. P. 33
30 - T. Soler Do Santos C. Imediata microcirúrgica breast
Reconstrução autonomização preoperative com: case report
Brazilian Journal of Plastic Surgery Vol 23-No 3 / 2008. P. 73.
31 .- Net Dos Anjos, André Leal. Reconstrução gives região do
calcaneus. Brazilian Journal of Plastic Surgery Vol 23-No 3 /
2008. Pag.92.
32 .- M. Cunha Dos Anjos Neto. Two implants microcirúrgicos
Aplicação no service of plastic surgery da Universidade da
Bahia: ANALYSIS OF THE RESULTS and complicações. Brazilian
Journal of Plastic Surgery Vol 23-No 3 / 2008. Pag.112.
33 .- Hazani Ron, MD, Bradley K. Simultaneous Bilateral Breast
Reconstruction The Use of Tissue and Identical Twin autogenous
Isograft. Annals of Plastic Surgery • Volume 63, Number 5,
November 2009
34 .- A com dois Reconstrução retalhos oromandibular
microcirúrgicos complexa. Brazilian Journal of Plastic Surgery,
vol 24 - No1/2009, pages 11-21.
|
|
|
|